QUICK FACTS
At long last, as of January 19, 2021 (the most recent update to this web page), an increasing number of media outlets are offering much more accurate facts about SARS-CoV-2 and COVID-19 than they were initially, when this web page launched in early March. Many politicians and media outlets, however, are still doing a disservice to citizens everywhere by offering incomplete or inaccurate information based on a faulty or politically motivated understanding. There is also confusion and contradiction within and between the many health organizations and websites that offer data, analysis, and health recommendations. Social media has then amplified some of this contradictory or incorrect information. In answer to this confusing landscape, the following highlights what we know to date from multiple sources — the standard disclaimer that we must of course remain vigilant about educating ourselves and not trust any one source of information (including this one) applies. That said, the following details appear to be either well-supported or strongly suggested by evidence from credible sources at this time:
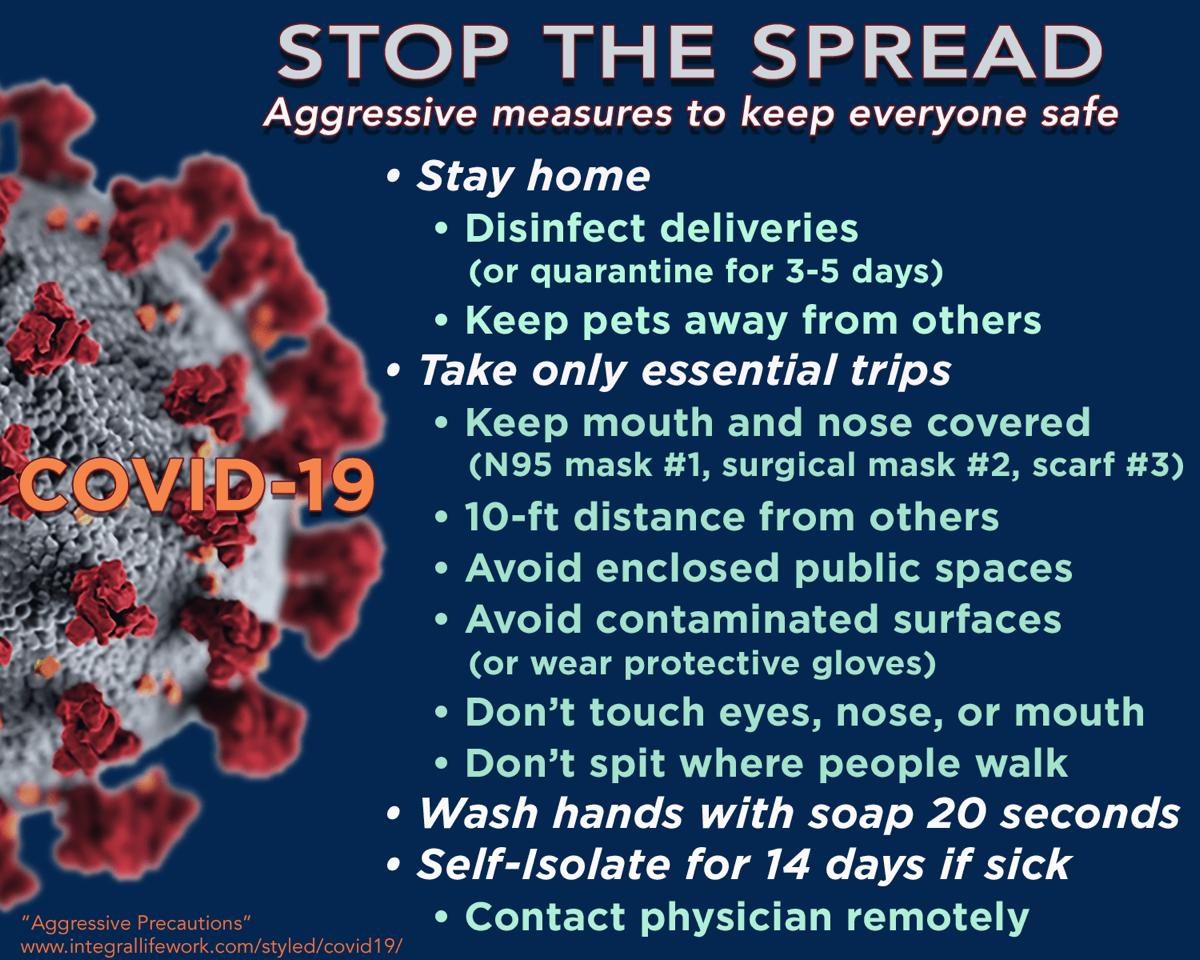
PRECAUTIONS
- Wear a mask. If it is possible that someone nearby may be infected with COVID-19 — or if we ourselves may have become infected — maintaining distance is likely not sufficient to avoid transmission. This is true both indoors and outside, but perhaps especially in enclosed interior spaces with recirculating air. Rapid implementation of collective mask wearing has quickly reduced spread in many countries (see Science Times article). Surgical masks, cloth masks with multiple layers, and of course N95 or N99 masks all are more effective than sheer, single-layer fabric face coverings (see Science Alert article and Duke University study). Some additional precautions due to N95 mask shortages and the need to re-use masks include: 1) Be careful not to self-contaminate when removing a mask or putting on a re-used mask, and wash hands afterwards. 2) Store reusable masks in paper bags after use so they can dry out, being careful not to contaminate the inside of the mask. Consider additional avenues of disinfecting the mask (spraying mask with disinfectant, rotating masks out for ones left unused for five days, etc.). Because of commercial N95 mask shortages, DYI mask-making in also an option (see: NY Post article and CDC 2006 letter DYI face mask prototype). An infected person can greatly reduce transmission by wearing such a mask, as well as protect themselves from infection. One last (important) consideration: Most masks with breathing valves to ease exhalation do not filter exhaled air, so wearing an additional cloth or surgical mask over the valved mask will better protect others.
- Get vaccinated. As of this writing, there are two EUA vaccines beginning distribution in the U.S., and several more completing clinical trials. There is every reason to be vaccinated against COVID-19, and very low risks for taking the vaccine. (see NYT Vaccine Tracker for additional info)
- Cooperate with social distancing measures, especially if “community spread” is already occurring. Avoid crowded places, close conversations, and enclosed spaces; postpone travel, work from home, and abide by restrictions from public officials.
- Avoid touching own eyes, nose, and mouth as much as possible.
- Eye protection. In situations where prolonged or close proximity exposure to airborne virus cannot be avoided (for example, in low-volume enclosed areas, or when near a talking/coughing person who is infected but not wearing a face mask), and especially for those who have underlying health conditions that place them in higher risk categories, a face shield or swimming goggles are advised to prevent airborne virus from contacting the eyes. See this WebMD article.
- Disinfect surfaces that may have been exposed. Many surfaces can transmit the virus for three days or more — possibly even items purchased in a store or shipped over distance. To disinfect hard nonporous surfaces, wipe down with a 1:40 bleach solution, 70% isopropyl alcohol, or disinfectant wipes (which must contain alcohol). Non-chlorine bleach (hydrogen peroxide) can also be used if it is sprayed on and allowed to dry (don’t wipe). See this CDC link for additional disinfecting information.
- Avoid physical contact with anyone who might be infected. Shaking hands, hugging, touching, kissing, sharing food and drink, and other intimate contact can transmit the virus. Remember that someone can be contagious without showing symptoms.
- Clean hands thoroughly after being in public, contact with animals or pets, contact with possibly contaminated surfaces — or after coughing, sneezing, or blowing your nose. Either wash with with soap and water for 20 to 30 seconds, or use hand sanitizer or wipes with at least 60% alcohol. See this helpful handwashing video.
- Wear gloves when in direct contact with someone who is infected, or when in direct contact with surfaces that may have been contaminated. Be careful not to self-contaminate when removing gloves, and wash hands afterwards.
- Avoid spitting onto any surface where someone else might walk, and be conscious of contaminating own shoes. It may be prudent to remove shoes worn in public places when re-entering one’s own living space.
- When someone has symptoms, they should self-isolate, consult medical professional over the phone or via a virtual checkup, and continue to wear a mask when around others — even after symptoms lessen or cease. Here again, a 14-day “self-quarantine” is recommended. It is important not to overwhelm medical facilities by showing up to an ER or Urgent Care facility for milder symptoms — the hospitals need to be able focus on acute interventions for the most serious cases.
TRANSMISSION
- Someone who is infected can transmit virus without showing symptoms. The incubation period of COVID-19 averages about five days. For 97% of patients, symptoms appear within 11 days. During this initial period, before and at onset of initial symptoms, the virus is the most contagious. This is one reason quarantine after suspected exposure to the virus lasts for 14 days.
- Most transmission appears to occur via droplets that are exhaled or coughed by an infected person. Because those droplets may be inhaled by someone, this resulted in the six-foot (two-meter) distance rule. However, droplets will also settle onto surfaces, which then transfer them to anyone who touches those surfaces — who then infect themselves by touching their eyes, nose or mouth.
- More extensive airborne (short-range aerosol) transmission has been documented. Evidence suggests that aerosols containing virus can persist over distance and remain in enclosed areas for up to three hours after an infected person has left the area. Therefore six feet (two meters) is insufficient distancing for some situations, and perhaps especially in low-volume interior spaces, or where air is being circulated without filtration.
- Surfaces can harbor virus for several days. On surfaces that have not been disinfected after exposure to droplets containing virus, SARS-CoV-2 can survive for three days, and possibly longer. This includes items frequently handled in retail environments, which should be quarantined or disinfected. However, this type of “fomite transfer” does not appear to be a primary source of transmission. That said, there is particular concern over public restrooms.
- Refrigeration or freezing can extend viability of coronavirus. SARS-CoV-2 can remain viable in cold environments for extended periods of time. The storing and consuming of cold food items should be handled with care and with appropriate food hygiene, and raw or undercooked animal products should be avoided.
- Bodily excretions can contain coronavirus. There is some evidence that COVID-19 could spread
- How contagious is COVID-19 — the reproduction ratio (R0) of the virus. SARS-CoV-2 has an R value of between 2 and 2.6, depending on measures taken to suppress transmission. For comparison, the median R value for influenza is about 1.28. Essentially, then, COVID-19 is twice as contagious as the flu.
- Receiving the COVID-19 vaccine does not necessarily prevent contagiousness of the person vaccinated. Those who receive the COVID-19 vaccine should continue the same precautions (wear a mask, social distance, etc.) because vaccines vary in their ability to prevent active virus from being transmitted by the person who is vaccinated. Read more in this Medscape article and NY Times article.
- There are indications that viral dosing may impact the severity of illness. There are indications that more frequent and prolonged the exposure to the virus, the more severe the contracted illness may become. See this NY Times article for discussion of “high-dose infection.” This has resulted in recommendations regarding length-of-exposure in various situations. However, at this time medical experts caution that we do not yet know what the “infectious dose” of SARS-CoV-2 actually is — and that it may in fact be quite low.
- This blog post by immunologist Erin Bromage provides a helpful overview of many of these transmission risks.
COURSE OF SYMPTOMS
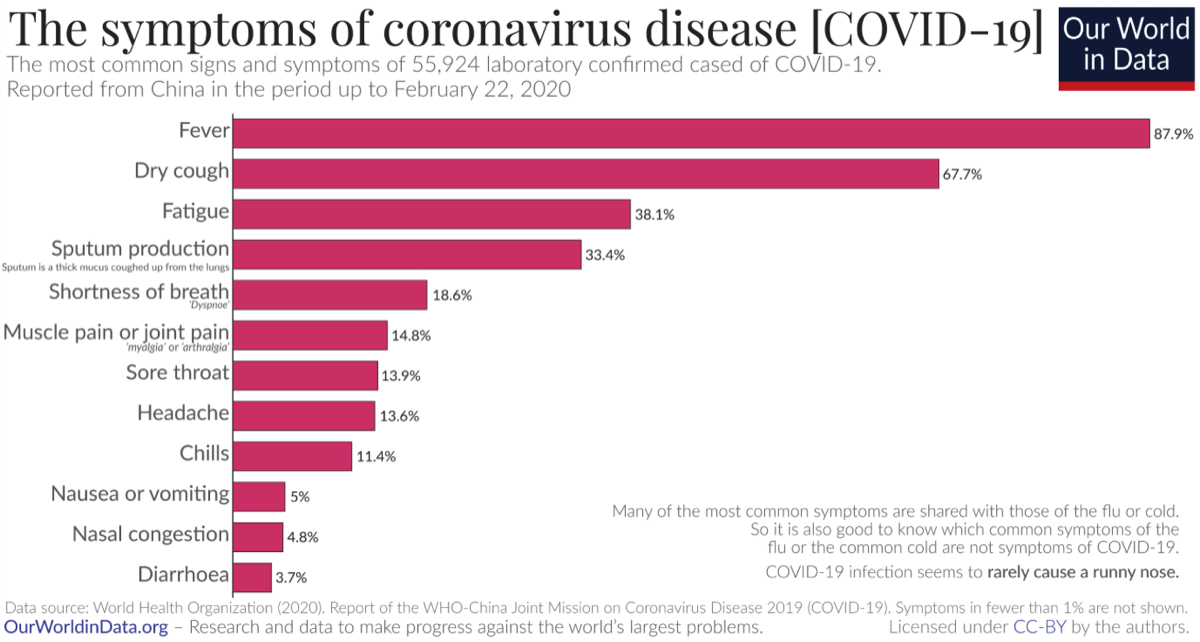
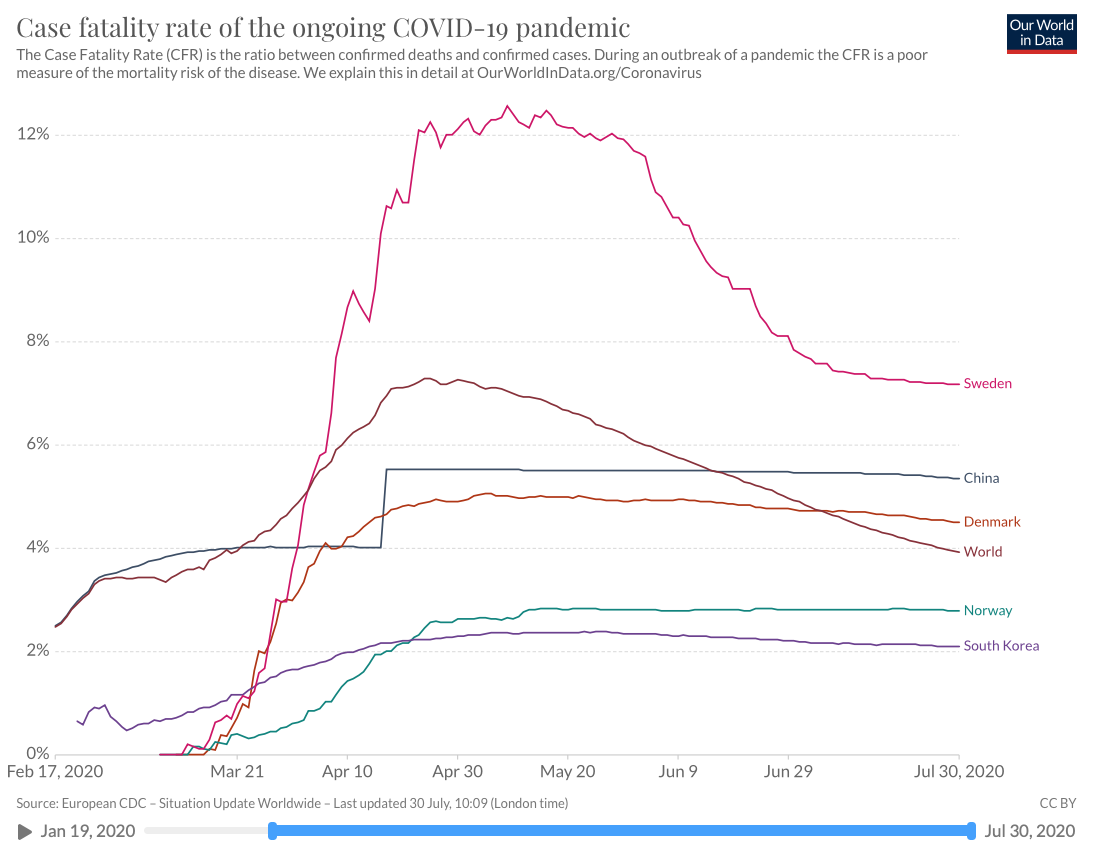
The adjacent chart is courtesy of ourworldindata.org using data from the World Health Organization.
The adjacent chart is courtesy of ourworldindata.org using data from the World Health Organization.
- Most symptoms begin between two days to two weeks after exposure.
- 81% of COVID-19 cases studied in China experienced mild symptoms.
- Roughly 25% of those contracting COVID-19 may have no symptoms at all, but still be contagious.
- A loss of smell or taste may be an early symptom of COVID-19. (More study needed.)
- Various symptoms, including soar throat, chest pains, fatigue, headache and intestinal upset/diarrhea have been reported at initial onset. (However, presentation is not consistent.)
- Fever usually occurs within an average of five days. (The fever may be mild.)
- Dry cough and fatigue within an average of five days.
- Difficulty breathing within an average of eight days.
- Potential onset of pneumonia/pneumonitis within an average of nine days.
- In the most severe cases, a “cytokine storm” has resulted in acute lung injury (ALI), acute respiratory distress syndrome (ARDS), respiratory failure, heart failure, sepsis and cardiac arrest.
- 10-12% of COVID-19 cases have required hospitalization, with 3-5% in ICU. (There are some indications that increased/repeat exposure resulting in higher viral dosing leads to more severe illness.)
- Resolution of symptoms may take 10-14 days for mild cases, and up to several weeks for more serious cases.
- ***Even cases with mild symptoms*** may experience blood clots that can lead to stroke or pulmonary embolism — as well as kidney, heart, liver, neurological, or brain damage. (More about these consequences here: UCL study, Medscape article, JASN article, AMJC article, Stat News article)
- There are increasing reports of a multi-system inflammatory syndrome in children and infants that appears to be linked to a previous infection with COVID-19, but may occur whether a patient tests positive or negative for coronavirus. This is similar to Kawasaki disease, and presents with fever, abdominal pain, rash or skin coloration, persistent fever, and difficulty breathing. (There is speculation that this may be clinical sequelae of the coronavirus, and has resulted in cardiac arrest and death in some children.)
- There is also a growing awareness of cases among otherwise healthy people where debilitating symptoms persist over 75 days. (See this Nature article and this Harvard article for discussion of these “long-hauler” cases. Another name for this is “post-viral syndrome,” since tests for COVID-19 may return negative results. See this NYT article for one such story.)
- This Science article offers an excellent overview of how COVID-19 attacks many organs and tissues in the body.
Healthcare professionals may want to consider reviewing these ER MD clinical notes from 3/30/20.
RISKS
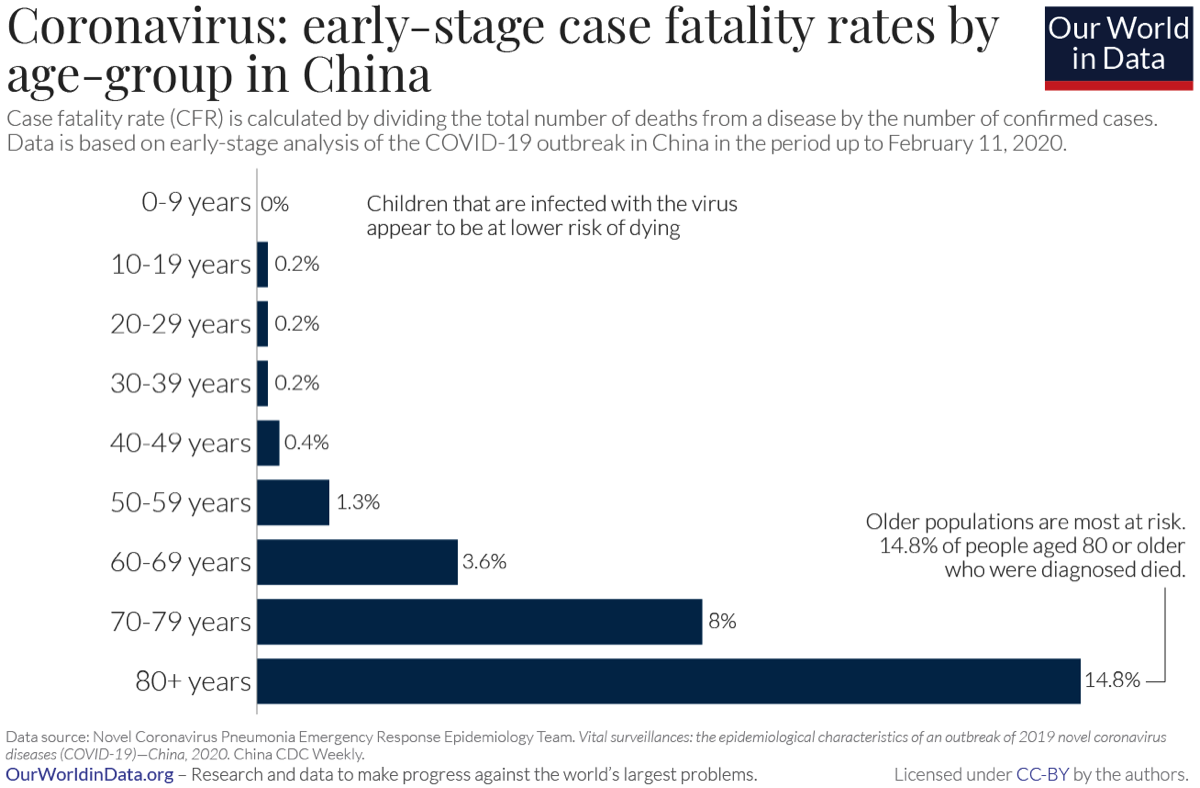
Mortality risks vary by age and pre-existing health conditions. The adjacent chart is courtesy of ourworldindata.org, using data from China CDC Weekly.
Chronic health conditions that increase risk include:
Other risk factors may include having a A or AB blood type (see SciTech Daily article).
Mortality risks vary by age and pre-existing health conditions. The adjacent chart is courtesy of ourworldindata.org, using data from China CDC Weekly.
Chronic health conditions that increase risk include:
- Diabetes
- Obesity (BMI > 29.9)
- Weakened immune system
- Lung disease
- COPD
- Cardiovascular disease
- High blood pressure
- Heavy smoking/vaping
- Other chronic illness
Other risk factors may include having a A or AB blood type (see SciTech Daily article).
In general, of the 10-12% of COVID-19 cases that required hospitalization, 40% have been age 20-54.
It is unclear at this time if an initial COVID-19 infection guarantees immunity from re-infection. Their have been cases (see Forbes article and Tech Times “reactivation” article) of apparent re-infection after initial recovery, but more study is needed. There are also indications that coronavirus immunity may, at best, only last for six months (see Science Times article).
Exposure to polluted air (high PM 2.5 levels) increases COVID-19 severity and mortality. See Science of the Total Environment article, Harvard study, The Conversation article
COVID-19 causes coagulation and inflammatory damage to the body’s organs and nervous system, with or without the involvement of severe respiratory symptoms. This damage can result in death or long-term health issues. Some findings are discussed here: UCL study, Medscape article, JASN article, AMJC article, Stat News article
It is unclear at this time if an initial COVID-19 infection guarantees immunity from re-infection. Their have been cases (see Forbes article and Tech Times “reactivation” article) of apparent re-infection after initial recovery, but more study is needed. There are also indications that coronavirus immunity may, at best, only last for six months (see Science Times article).
Exposure to polluted air (high PM 2.5 levels) increases COVID-19 severity and mortality. See Science of the Total Environment article, Harvard study, The Conversation article
COVID-19 causes coagulation and inflammatory damage to the body’s organs and nervous system, with or without the involvement of severe respiratory symptoms. This damage can result in death or long-term health issues. Some findings are discussed here: UCL study, Medscape article, JASN article, AMJC article, Stat News article
WHY TAKING PRECAUTIONS IS IMPORTANT
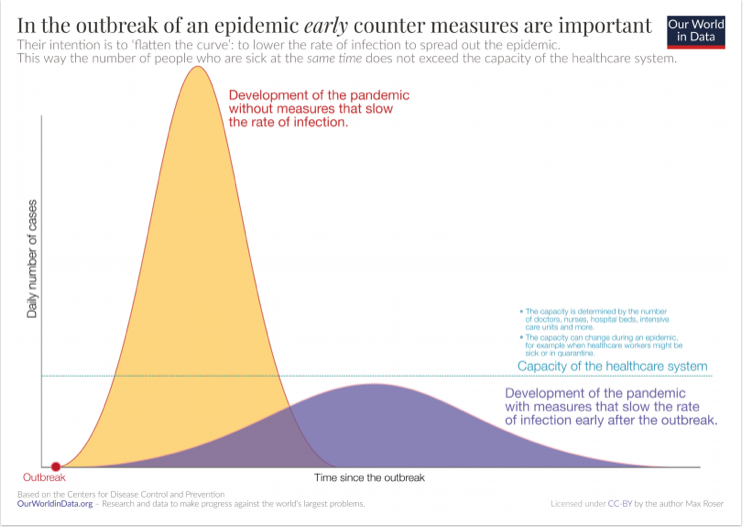
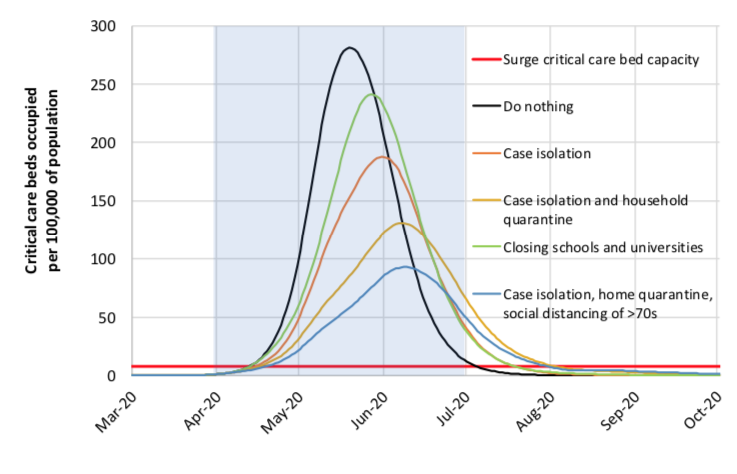
Reducing impact on health care system. The adjacent chart from ourworldindata.org (CDC projections) shows the potential difference taking precautions can make on the rate of new infections — which then translates into the number of urgent cases that hospitals and clinics will have to manage at one time. The goal is to “flatten the curve” of that impact, and stretch it out over time.
Reducing impact on health care system. The adjacent chart from ourworldindata.org (CDC projections) shows the potential difference taking precautions can make on the rate of new infections — which then translates into the number of urgent cases that hospitals and clinics will have to manage at one time. The goal is to “flatten the curve” of that impact, and stretch it out over time.
Preventing infection of vulnerable and high risk. Everyone taking precautions helps protect those over sixty or who have preexisting health conditions, where symptom severity and mortality rate are potentially much higher. However, the 10-12% of cases that become more serious can impact everyone across all age ranges and health conditions, so at this time the concern is really about protecting everyone from harm.
Avoiding long-term health impacts — even in COVID-19 cases with less severe symptoms. There is increasing concern that severe COVID-19 symptoms are not the only risk when contracting the virus. There is increasing evidence that other long-term health impacts can result from contracting COVID-19. These range from kidney, heart and lung damage to strokes, neurological problems and psychological impacts. As just one example, a recent study indicates that over half of those that recovered from COVID-19 suffered from increased levels depression, anxiety, and PTSD — possibly a consequence of the inflammation caused by COVID-19 (see this Guardian article).
UNDERSTANDING MORTALITY RATE
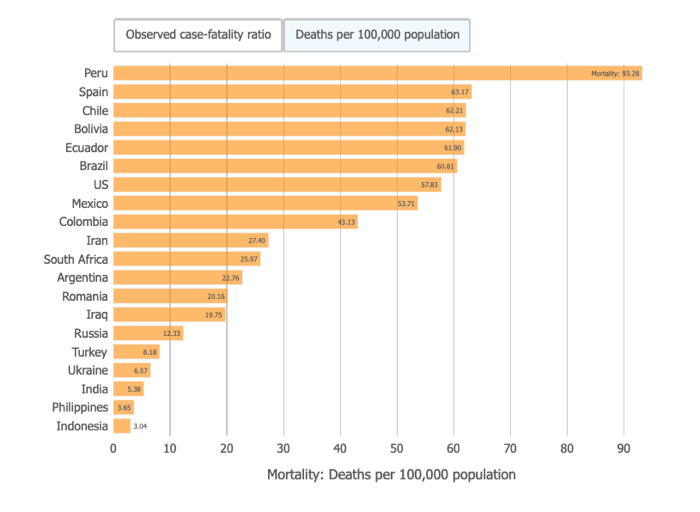
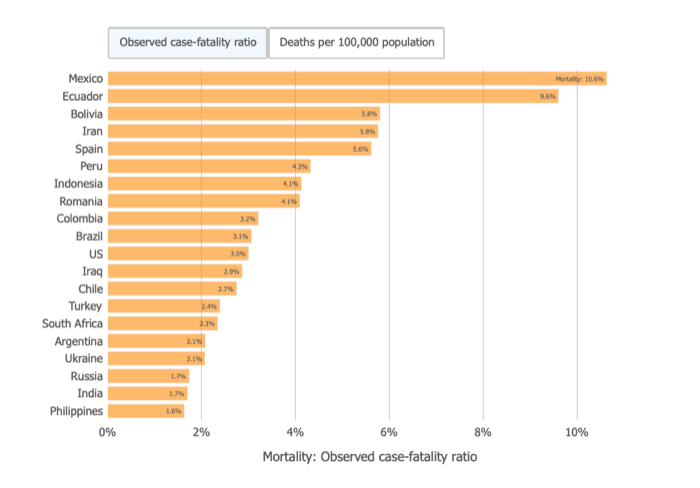
The per capita mortality rate and case fatality rate will always be different that the total mortality rate. Basically they are illustrating how many people are dying out of either every 100 confirmed cases (case fatality rate) or per 100,000 in population (per capital mortality rate).
The per capita mortality rate and case fatality rate will always be different that the total mortality rate. Basically they are illustrating how many people are dying out of either every 100 confirmed cases (case fatality rate) or per 100,000 in population (per capital mortality rate).
TESTING,TREATMENT & MITIGATING NEGATIVE IMPACTS
TESTING & TREATMENT
- There is no universally recommended treatment for COVID-19 at this time. Importantly, many supposedly effective treatments that are circulating on social media (sipping water frequently, gargling with salt water, taking extra vitamin C or A, blowing hot air up nose, etc.) are actually not effective.
- Testing is critical to understanding COVID-19 spread and containment, but where supplies are limited (most notably in the U.S.) only those with symptoms and whose physician recommends testing will receive a test. There have been issues with false negatives with some early PCR tests, as well as a processing bottleneck at labs that have delayed the normal 24-hr turnaround time, but additional molecular tests are in development and molecular PCR is currently the most reliable test method. Rapid antibody testing using lateral flow immunoassay technique is another promising test method as well, and several antibody tests are under development and testing. You can read about these efforts here: Nature article.
- Under FDA Emergency Use Authorization (EUA), rapid molecular testing at point-of-care (“POC diagnostics”) became available in late March, 2020. Rapid RT-PCR and isothermal nucleic acid amplification are two point-of-care methods that can provide results in under 30 minutes. Companies that have received COVID-19 EUA authorization are listed here: FDA EUA
- One promising approach is the prioritization and widespread implementation of “contagiousness testing.” The idea here is to focus on indicators of contagiousness, such as the “e25” test that is keyed to the SARS-CoV-2 spike protein, via simple, cheap, paper strip tests that everyone could self-administer using a saliva sample. You can read more about this here: Atlantic article.
- A number of vaccines are completing clinical trials — and EUAs have been issued for Pfizer and Moderna vaccines that are up to 95% effective — and an increasing number will become available in the coming months (see NYT Vaccine Tracker).
- Remdesivir has completed clinical trials, but efficacy remains questionable, resulting in only slight improvements in symptoms. Other drugs that initially showed promise in treating COVID-19 were Favilavir/Avigan and chloroquine/hydroxychloroquine, but these have been disappointing as well. Initially, it was thought that the anti-inflammatory Tocilizumab, which targets IL-6 receptors, would be helpful, but trials have shown it to be ineffective for serious cases (see NEJM article) and it has some unfortunate side effects (see STAT article).
- A hydroxychloroquine + azithromycin combination initially indicated reduction in viral loads of SARS-CoV-2, prompting clinical trials evaluating efficacy (See: Science Direct article and Clinicaltrials.gov) However, evidence for using the anti-malarial drugs hydroxychloroquine/chloroquine alone to treat COVID-19 was always minimal, and clinical trials and field data have since demonstrated they are not effective in reducing mortality, and in fact can induce life-threatening side-effects (see FDA overview). One larger VA had also indicated increased lethality using the anti-malarial drug (see VA Study), and several additional studies have shown no benefit in treating COVID-19 (see Science magazine article). Both the antimalarial’s use alone, and in combination with azithromycin, can result in cardiac and pulmonary complications (see: Cardiology article), and the combination has so far not demonstrated any positive impact on mild to moderate COVID-19 cases (see NEJM article). The prophylactic efficacy of hydroxychloroquine/chloroquine has also been evaluated, and it also does not appear to prevent contracting COVID-19 (see NEJM article).
MITIGATING NEGATIVE IMPACTS
(on economy and society)
(on economy and society)
- Cultures and regions that have reacted swiftly, collectively and uniformly to COVID-19 have been the most successful at eliminating local transmission. Several regions in Asia have been able to rapidly contain infection rates — though those measures will have a major impact on economic productivity.
- Testing anyone who has been exposed, and then tracking all of their movements and interactions, has allowed effective targeting of containment measures. Here again Asia has led the efforts to “test and track.” For example, China and South Korea have utilized smartphone apps to gather data and notify citizens and services about each individual’s level of risk and safety, and developers in other countries are now working on equivalent smartphone utilization (see: Wired article).
- Many governments are implementing massive economic stimulus packages to cushion the the economic damage and hardships created by COVID-19. At this time, it is unclear if these efforts will slow a global recession, restore lost jobs and reopen closed businesses, or otherwise reverse the downward spiral.
- Where available, efforts are being made to continue K-12 and higher education via virtual classrooms all around the globe.
- Expanded use of the Internet is also allowing those under “stay at home” isolation orders to work remotely, participate in virtual gym workouts, order grocery and meal deliveries, and remain socially and culturally engaged.
NEW ENGLAND JOURNAL OF MEDICINE:
NO BENEFIT FROM HYDROXYCHLOROQUINE WITH OR WITHOUT AZITHROMYCIN
NO BENEFIT FROM HYDROXYCHLOROQUINE WITH OR WITHOUT AZITHROMYCIN
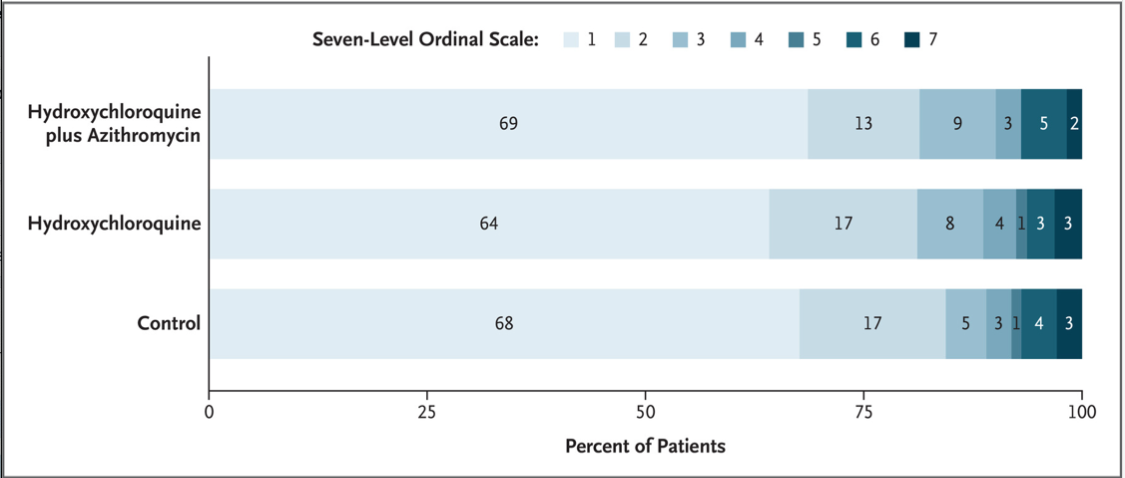
- The primary outcome was clinical status evaluated at 15 days according to a seven-level ordinal scale. The scores on the scale were defined as follows: a score of 1 indicated not hospitalized with no limitations on activities; 2, not hospitalized but with limitations on activities; 3, hospitalized and not receiving supplemental oxygen; 4, hospitalized and receiving supplemental oxygen; 5, hospitalized and receiving oxygen supplementation administered by a high-flow nasal cannula or noninvasive ventilation; 6, hospitalized and receiving mechanical ventilation; and 7, death. The percentages shown have been rounded to whole numbers. (From: https://www.nejm.org/doi/full/10.1056/NEJMoa2019014)
- Revisiting the time-proven technique using blood plasma from survivors of COVID-19 could provide both immunity and speed healing in the infected. Plasma-derived therapy was used early on in China to combat COVID-19, and improved techniques under development could be fast-tracked for approval in the U.S. The FDA currently offers a pathway for emergency investigative use for convalescent plasma (see FDA overview).
- Along similar lines to plasma, synthetic antibodies have also shown promise, and may both accelerate recovery and prevent infection. (see Science article and this news article). Most recently, two monoclonal antibodies — casirivimab and imdevimab — were approved for emergency use by the FDA (see FDA announcement).
- Dexamethasone (and other corticosteroids like it) can potentially reduce mortality in the most serious COVID-19 cases by up to 30%. However, there was no benefit for non-serious cases — that is, for those that did not require supplemental oxygen or mechanical ventilation, dexamethasone did not improve outcomes (see NIH overview).
- In the most severe cases, cytokine storm may potentially be attenuated by the use of 3 to 10mg/day melatonin. Melatonin’s reduction of pro-inflammatory cytokines could make it a candidate for adjuvant treatment for COVID-19. See this Life Sciences article.
- Most patients with mild symptoms (81%) appear to recover on their own.
- 10-12% of those infected require hospitalization due to more serious symptoms and 3-5% require ICU. Some 40% of those hospitalized have been age 20 to 54.
- The most serious COVID-19 cases require a respirator.
- There are some indications that fluids (even maintenance fluids) in severe cases may increase risk of pulmonary or cardiac complications.
- There was initially an hypothesis that NSAIDS (like ibuprofen and aspirin) could worsen COVID-19 infection or lower the body’s natural immune response — however, there has been no data to confirm this hypothesis. Contrary to this hypothesis, there is a competing theory that 100mg/day of aspirin may have multiple positive impacts on COVID-19 infection. There are currently clinical trials to test the safety and efficacy of aspirin.
- Proning patients (turning onto stomachs) appears to be an effective way to improve breathing for patients suffering from ARDS.
- There are also currently clinical trials underway to evaluate the effectiveness of nitric oxide, which appears to assist with oxygenation, slow coronavirus replication, and speed up healing. See this Medpage Today article.
- For additional information on COVID-19 research, please see this Nature article, and read about the latest COVID-19 treatment news here.
Healthcare professionals please consider reviewing these ER MD clinical notes from 3/30/20.
DURATION OF COVID-19 DISRUPTION TO SOCIETY
SUPPRESSION EFFORTS
To control spread and reduce fatalities, some combination of mitigation (masks, social distancing) and suppression (collective stay-at-home/lockdown compliance) will likely be needed for up to 18 months. The adjacent charts from an Imperial College COVID-19 Response Team study indicate how different strategies impact fatalities and ICU demand over time — with the clear indication that even aggressive measures will require repeat application until vaccines become more widely available to avoid new outbreaks of COVID-19. Alternatively, if an effective treatment is made widely available that can relieve symptoms and prevent hospitalization, this has the potential of reducing disruptive social and economic impacts.
To control spread and reduce fatalities, some combination of mitigation (masks, social distancing) and suppression (collective stay-at-home/lockdown compliance) will likely be needed for up to 18 months. The adjacent charts from an Imperial College COVID-19 Response Team study indicate how different strategies impact fatalities and ICU demand over time — with the clear indication that even aggressive measures will require repeat application until vaccines become more widely available to avoid new outbreaks of COVID-19. Alternatively, if an effective treatment is made widely available that can relieve symptoms and prevent hospitalization, this has the potential of reducing disruptive social and economic impacts.
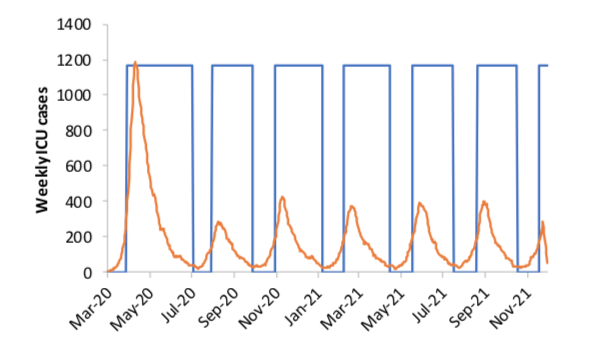
In the second chart, the orange line represents new ICU cases, and the blue line represents repeat triggering of suppression strategies (quarantine, social distancing, school closures, etc.) whenever ICU cases begin to spike.
Ongoing efforts to carefully pace and monitor opening things back up after lockdown periods will be critical to mitigating disruption to society. Here are some recommendations on how best to approach this:
Ongoing efforts to carefully pace and monitor opening things back up after lockdown periods will be critical to mitigating disruption to society. Here are some recommendations on how best to approach this:
- CDC COVID-19 planning and cleaning recommendations for reopening workplaces, public spaces, schools, etc.
- WHO publications on reducing COVID-19 risks in workplaces, schools, hotels, long-term care facilities, etc.
REOPENING AFTER LOCKDOWN
Reopening both communities and schools after lockdown has been challenging and unpredictable. As the Imperial College study above suggested, it will be extremely difficult to control or contain the virus until a vaccine has been developed. Nearly everywhere reopening has been attempted after COVID-19 infection rates were greatly reduced, results have been mixed — sometimes seeming to be almost arbitrary — when SARS-CoV-2 is reintroduced into those populations. Some of the reasons for this variability include:
These considerations apply to all reopening scenarios, including the reopening of schools. Even so, there have been examples where every possible precaution has been taken, but COVID-19 nevertheless surged back in community spread. Here are some instructive examples:
Reopening both communities and schools after lockdown has been challenging and unpredictable. As the Imperial College study above suggested, it will be extremely difficult to control or contain the virus until a vaccine has been developed. Nearly everywhere reopening has been attempted after COVID-19 infection rates were greatly reduced, results have been mixed — sometimes seeming to be almost arbitrary — when SARS-CoV-2 is reintroduced into those populations. Some of the reasons for this variability include:
- Indications that those infected with the virus are most contagious before symptoms (such as elevated temperature) are present (see Science News article).
- How diligently everyone — including children — can follow infection reduction guidelines (masks, hand washing, distancing, etc.).
- Opening up travel restrictions allowed those returning to communities from abroad can reintroduce virus.
- The ability to aggressively and swiftly test and contact trace whenever a new outbreak arises.
These considerations apply to all reopening scenarios, including the reopening of schools. Even so, there have been examples where every possible precaution has been taken, but COVID-19 nevertheless surged back in community spread. Here are some instructive examples:
- Resurgence of COVID-19 in Asia and the Pacific, where virus had been contained, after reopening.
- Relaxing of travel restrictions in Asian countries leads to new outbreaks.
- School reopenings around the world model how dynamic and flexible the process has to be be — rather than a “one size fits all” solution.
- U.S. States where schools closed in Spring of 2020 had the best overall reduction in COVID-19 infections and deaths.
- Challenges to school reopening in Israel
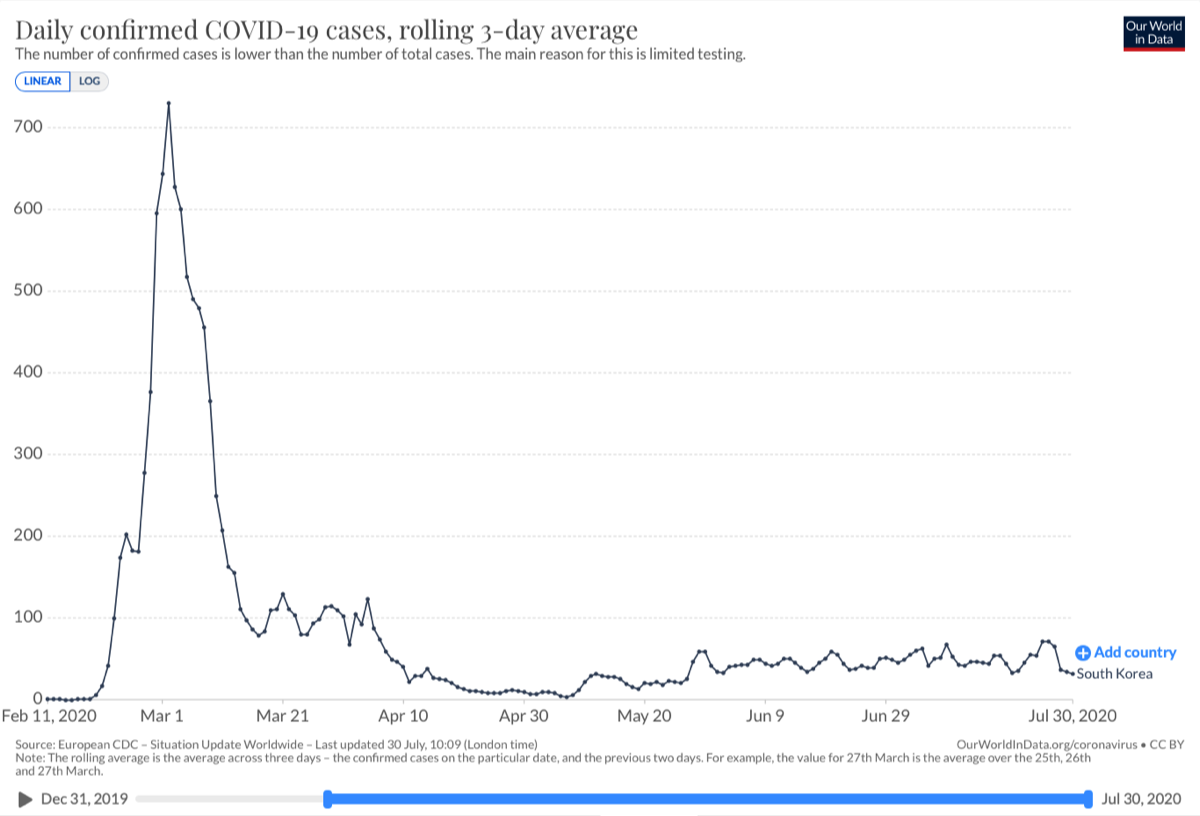
ADVANTAGES OF INCREASED TESTING AND MONITORING — SOUTH KOREA
It is possible to relax suppression measures more quickly with the right testing, tracking and prevention strategies. Evidence from South Korea indicates that the right testing, tracking and prevention approaches could allow a more rapid return-to-normal and ongoing infection management. For example, not only can anyone and everyone in South Korea be tested at pop-up mobile facilities — and receive their results in 12 hours — but pharmacies have provided South Koreans up to two face masks per person per week. However, it is not clear that these measures alone will prevent a resurgence of infections; they may perhaps only allow a quicker relaxation of social distancing, quarantine, schools closures, and other suppression measures. See Science article on South Korea’s strategy and results. Also consider reading this STAT article that compares different approaches around the globe.
It is possible to relax suppression measures more quickly with the right testing, tracking and prevention strategies. Evidence from South Korea indicates that the right testing, tracking and prevention approaches could allow a more rapid return-to-normal and ongoing infection management. For example, not only can anyone and everyone in South Korea be tested at pop-up mobile facilities — and receive their results in 12 hours — but pharmacies have provided South Koreans up to two face masks per person per week. However, it is not clear that these measures alone will prevent a resurgence of infections; they may perhaps only allow a quicker relaxation of social distancing, quarantine, schools closures, and other suppression measures. See Science article on South Korea’s strategy and results. Also consider reading this STAT article that compares different approaches around the globe.
July 30, 2020 summary South Korea’s success. The adjacent graph from Our World in Data shows how effective South Korea’s approach COVID-19 has been. Date range: February 11 — July 30, 2020
VERTICAL INDERTICTION PROPOSAL
A “vertical interdiction” alternative that targets high risk populations is another (controversial) option. As proposed by David L. Katz, the idea would be continuously isolate only those with the highest risk factors (“especially vulnerable,” EV), while allowing lower-risk populations to return to work and school after a period of self-isolation and symptom resolution that clears them of being contagious. This approach could also potentially offer a more rapid return-to-normal, but it is dependent on several factors, including the following:
And here are some additional questions and concerns raised in response to the vertical interdiction proposal:
I would further submit that piloting any such approach on a small scale, to see if it is actually workable, will be a critical first step….
A “vertical interdiction” alternative that targets high risk populations is another (controversial) option. As proposed by David L. Katz, the idea would be continuously isolate only those with the highest risk factors (“especially vulnerable,” EV), while allowing lower-risk populations to return to work and school after a period of self-isolation and symptom resolution that clears them of being contagious. This approach could also potentially offer a more rapid return-to-normal, but it is dependent on several factors, including the following:
- A more accurate understanding of who is really at highest risk for more serious symptoms and mortality.
- A more accurate understanding of mortality rates overall (Dr. Katz notably downplays data from Italy and elsewhere that suggest a higher mortality rate than initial data from China).
- Highly reliable and widely available tests (PCR, antibody, etc.) that can provide the ongoing data necessary for this scenario to work.
- Ongoing, regular monitoring efforts of the entire population (as is being done in China and South Korea) to track new vectors and outbreaks.
- Healthcare workers, routinely tested for COVID-19, who provide care preferentially to high risk populations.
- Confirmation of individual and herd immunity, duration of immunity, and non-transmissibility as conditions for ongoing implementation.
And here are some additional questions and concerns raised in response to the vertical interdiction proposal:
- It would require extensive systems to support the EV population and their immediate family, committed partners, and loved ones while in isolation — which would continue until effective treatments or vaccines become available. Without support that extends to all immediate significant relationships, vertical interdiction has the potential of permanently fracturing or injuring those relationships.
- There is the real potential for stigmatization of EV populations, and hostility toward them, as they become associated with social distancing, economic slowdowns, an increased cost burden to society, and with the coronavirus itself.
- The “who decides” problem: Will a faceless government agency make the EV designation, as well as who will be considered immediate family and loved ones? Will an overworked, highly stressed medical professional make this decision? An insurance company that is constrained by profit considerations? Will individuals and families have any say in the matter? This poses profound questions about both skillful care and fairness…but also raises issues of personal freedom and justice.
- What about undiagnosed EV populations — those whose chronic conditions are not well-documented or clearly identified (even to them)?
- And how can we avoid a deepening stratification of society between those who have the means, supportive relationships and privilege to weather their EV status in relative comfort, and those who lack the economic security, social capital or supportive relationships to do so?
I would further submit that piloting any such approach on a small scale, to see if it is actually workable, will be a critical first step….
SWEDEN’S “NO LOCKDOWN” HERD IMMUNITY APPROACH
Sweden attempted to avoid the worst economic consequences by promoting individual choice without any state-mandated lockdowns. Although we won’t know the ultimate consequences of this decision for some time, as indicated in the 07/30/2020 adjacent chart, the results have not been great. (Click on chart for most recent data.)
Sweden attempted to avoid the worst economic consequences by promoting individual choice without any state-mandated lockdowns. Although we won’t know the ultimate consequences of this decision for some time, as indicated in the 07/30/2020 adjacent chart, the results have not been great. (Click on chart for most recent data.)
- The graph above from Our World in Data illustrates the consequences of Sweden’s approach as compared to other countries. Date range: February 17 — July 30, 2020. In May, COVID-19 death rates in Sweden were more than ten times those of its neighbors, Norway and Finland. They have since decreased, but are still much higher than surrounding countries.
- About 30% of these deaths have occurred among the elderly.
- There is another notable statistical difference in Sweden: it is experiencing considerably more fatalities than recoveries from COVID-19.
- While personal spending in Sweden has decreased about half as much as neighboring countries, GDP is still expected to contract at about the same rate as other developed countries.
- Initially it was thought that Sweden’s population might be nearly a third of the way to achieving herd immunity, where 70% of the population would have antibodies to the initial strain of SARS-CoV-2. However, herd immunity is usually accomplished with the help of vaccines — especially if illness, disruption to society, and fatality rates are either high or catastrophic. Increasingly, evidence indicates that herd immunity may not be possible with this particular virus, as this article on a recent antibody study in Spain suggests.
- At the peak of infection, Sweden’s healthcare system was not overwhelmed, and was operating at about 80% capacity.
- So far, the trade-off for leaving much of the Swedish economy open has been clear: more people have died so far, and without a clear economic benefit to Sweden. We simply will have to wait to see how this strategy plays out over the next few months, but right now — especially in comparison to other, more successful strategies in other countries — it looks like Sweden made a mistake.
For more info, please see: Business Standard article; Thaiger article; AFR.com; Science Alert article on herd immunity
ORIGINS, SPREAD AND CHARACTERISTICS OF VIRUS
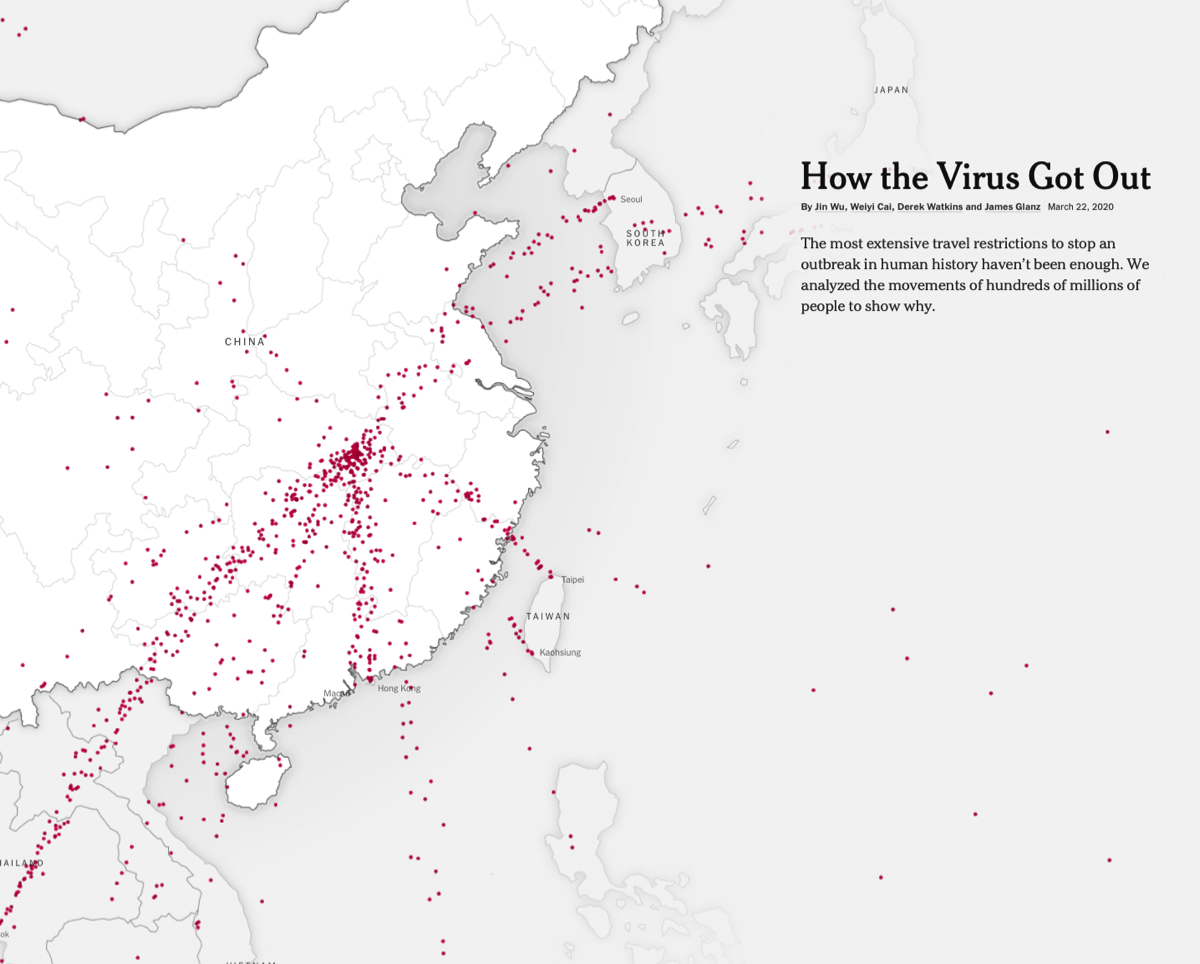
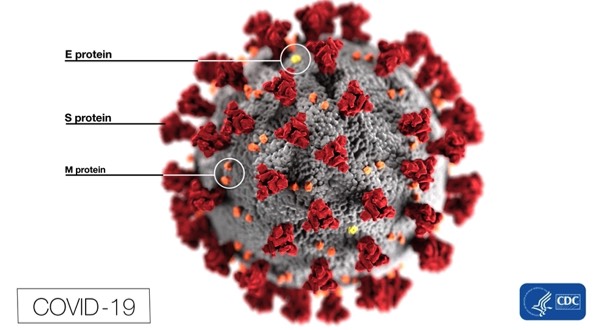
- COVID-19 is very likely a consequence of zoonotic spillover, which is caused by human incursions into natural habitats and increased interactions with new wildlife populations. Our understanding so far is that this novel coronavirus is a naturally occurring recombinant hybrid of strains originating in bats and pangolins — with a key contribution of the pangolin strain being a spike protein that interacts with proteins on human cells. It was then transferred to humans in a Wuhan, China wet market (adjacent image from Wikipedia article). The first human case could have occurred after exposure to the uncooked bodily fluids of an infected animal, likely while slaughtering it. There is a possibility that SARS-CoV-2 evolved into its pathogenic form after jumping to humans.
- COVID-19 spread so quickly because it went undetected and unmitigated throughout December, 2019 through January 23, 2020. Because of the extensive travel in China around the Chinese New Year, the virus spread quickly throughout the country prior to its discovery and the subsequent lockdown measures. International travel that spread the virus from China to other countries was also unrestricted for most of January. At this point containment was no longer possible, and most travel restrictions put in place around the world came too late. An animated map of the spread (pictured at right) can be viewed here: NY Times.
- COVID-19 became a pandemic because humans have no resistance to it, it is highly contagious, it produces a relatively low mortality rate, and many people do not present severe symptoms when infected. In other words, COVID-19 was able to spread quickly, without people even knowing they were carriers, prior to precautionary measures like social distancing.
- Conspiracy theories abound, of course. But there is no evidence to suggest, for example, that the novel coronavirus is an engineered bioweapon. In fact, there is increasingly clear evidence that it evolved in nature — see Science News article.
ADDITIONAL RESOURCES
HELPFUL LINKS
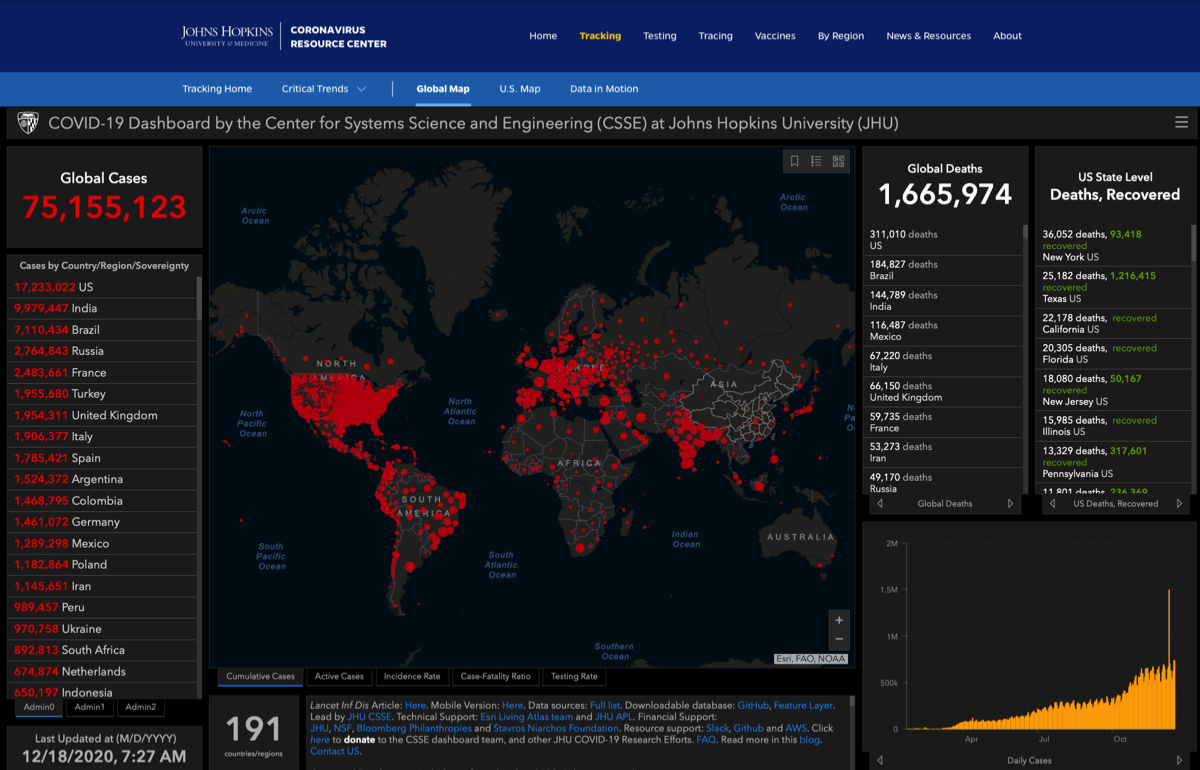
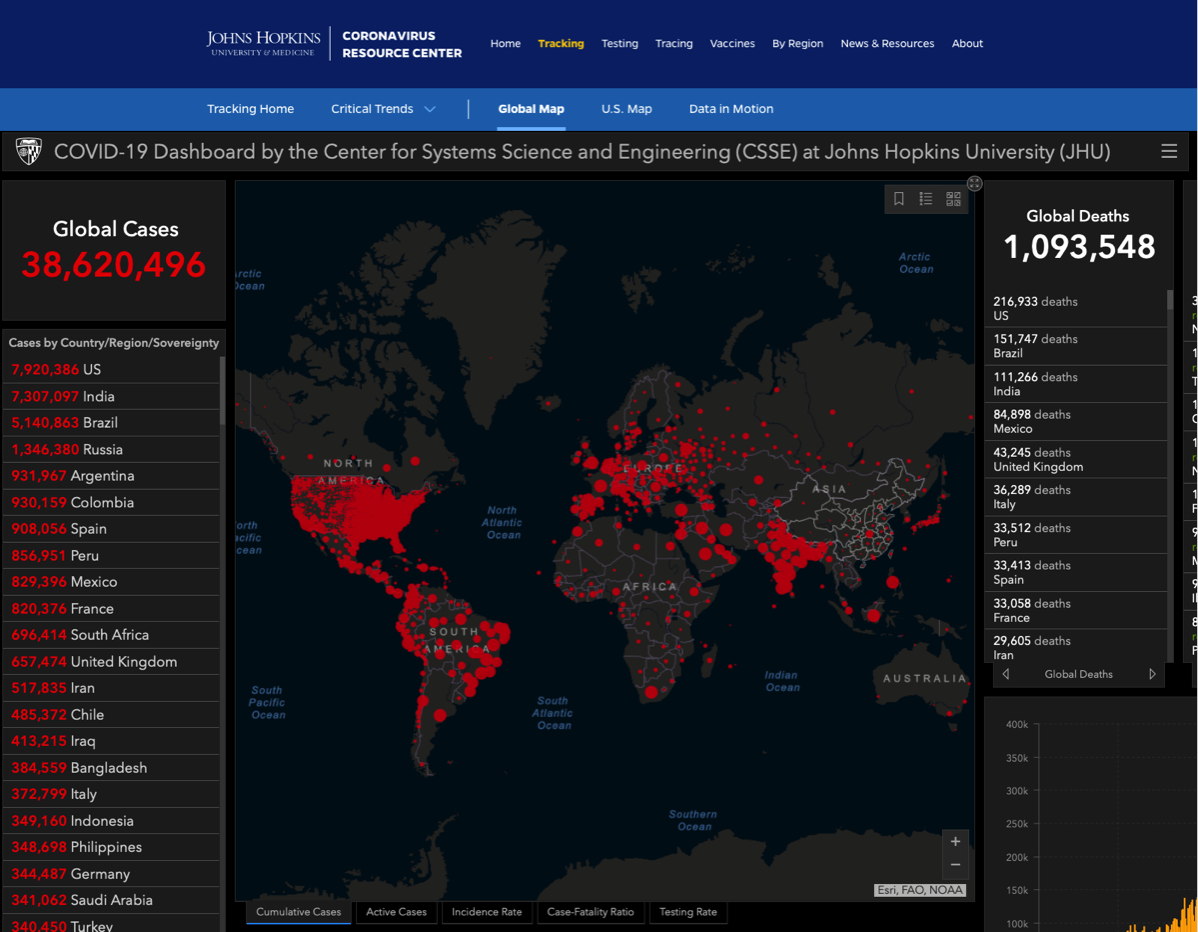
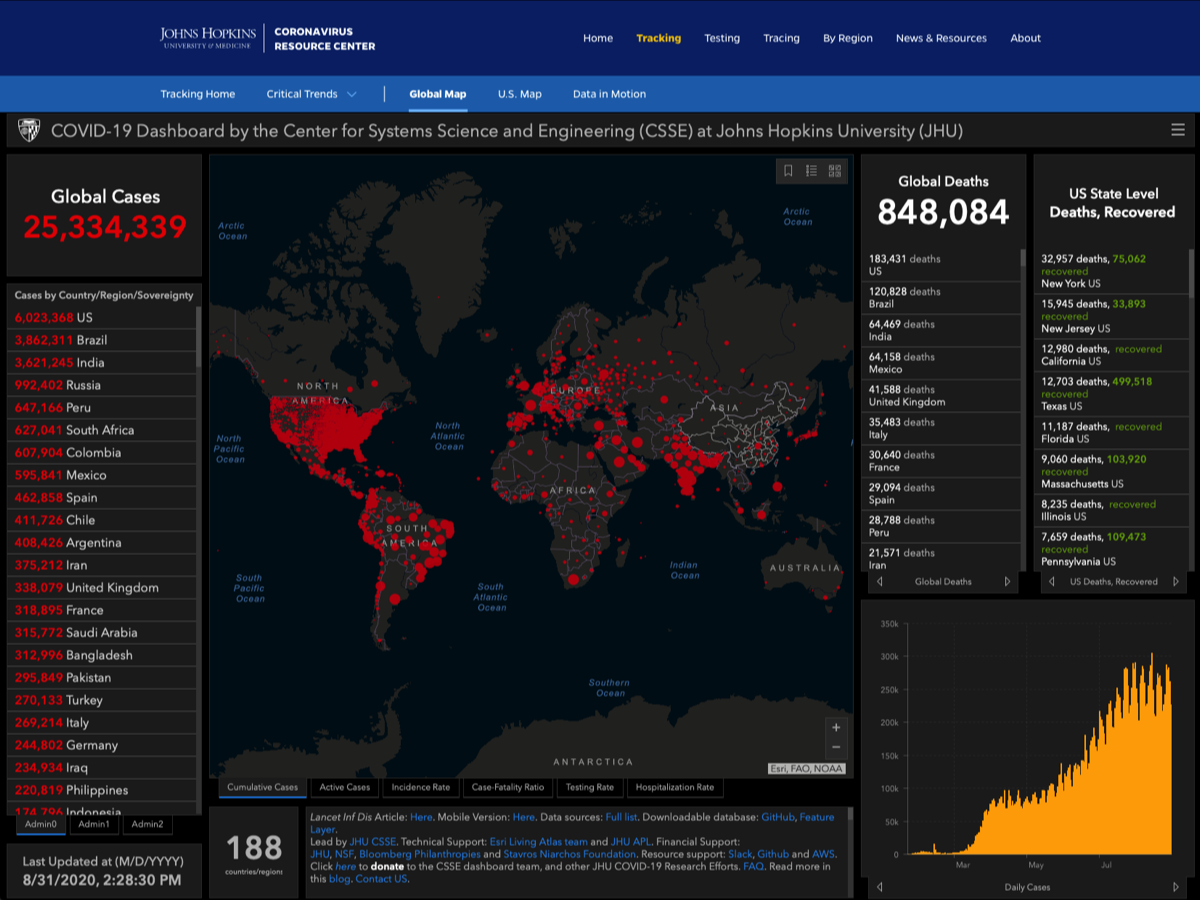
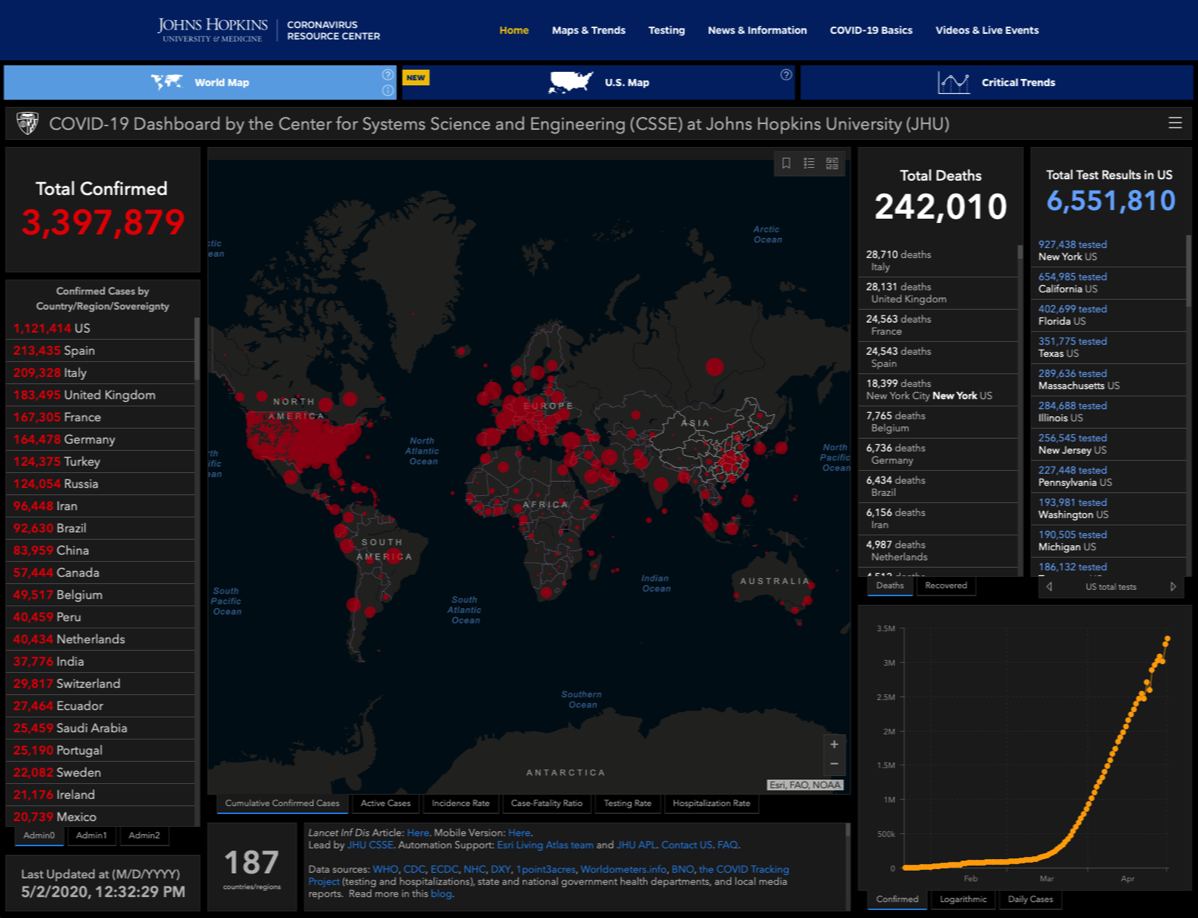
- Johns Hopkins COVID-19 Map global infection maps —>
- Updated Financial Times graphs & maps
- Latest Scientific Articles at Science News
- Airborne Transmission?
- Transmission via Aerosols & Surfaces
- NIH Vaccine Clinical Trial
- Incubation Period
- ARS Technica Overview
- Our World in Data
- Cleveland Clinic FAQ
- World Health Organization Info
- CDC Info
- WebMD Summary
- NIH Remdesiver Trial
- Questionable Efficacy for Hydroxychloroquine (Science)
- CPA NSAID Discussion
- Imperial College COVID-19 Response Team Study
- Comparing and Contrasting Containment Strategies (STAT)
- Forbes Article on Re-Infection
- Article on Zoonotic Spillover
- Video from Dr. Zubin Damania with Medical Advice for Health Professionals
- Emcrit.org COVID-19 Critical Care
- Antibody Testing (Science)
- Plasma-Derived Therapy (STAT)
- CDC Therapeutic Options Info
- ACE2 Discussion (Science Daily)
- Mutations and pathogenicity (Sky News)
- Scripps Research article on mutations and infection rates.
- An overview of how COVID-19 attacks organs and tissue throughout the body (Science)
- Proning patients (CNN)
- Multisystem inflammation in some children (Live Science)
- Nitric oxide & BCG (Medpagetoday.com)
- Pediatric multi-system inflammatory syndrome associated with COVID-19
- Possible dexamethasone breakthrough (BBC)
- Obesity and more severe COVID-19 (JHU)
- Airborne transmission update (The Atlantic)
- Increases in psychiatric disorders after COVID-19 recovery (The Guardian)